To understand autoimmune disease, it helps to first understand the meaning of the word autoimmune. Autoimmune can be broken down into two parts: auto, or “self,” and immune, the “immune system.” Autoimmunity is when the immune system attacks the body instead of protecting it. The body’s immune system is designed to protect the body and fight off infections. With an autoimmune disease, the body begins to attack its organs, tissues, cells, and cell components.
The body attacking itself is clearly not normal. But why does this happen? More importantly, what can be done about it? To find a viable solution, you have to have to get to the root of what it is and why it is happening.
The day you are born is pretty much when the immune system starts to form.
Consequently, things that occur very early on in life, like C-sections vs. vaginal births, or being bottle-fed versus breastfed, can have a meaningful impact on the health of the immune system. Knowing this, it is understandable that a mother’s health can play a major role in the healthy development of a robust immune system. Breastfeeding is key as breast milk supplies unique antibodies that contribute to a healthy immune system in infants.
Historically, children born to mothers with autoimmunity have tended to have a higher risk of developing autoimmunity. This is where genetics come into play. Genetics matter, but we are learning that genetic predispositions are somewhat malleable. You indeed have a higher chance of developing an autoimmune disease if it runs in your family. The good news is, we are learning more and more that just because autoimmunity is in your genes doesn’t mean you are destined to develop it or live with it. The study of epigenetics teaches us that we have the ability to “turn off” bad genes and “turn on” good ones. Epigenetic changes can alter the physical structure of DNA. So just because autoimmunity runs in your family doesn’t mean that you are doomed.
Your genes do predispose you to specific conditions, but epigenetics trigger the action.
Think of genetics as the gun. Epigenetics represent engaging the trigger. The gun can sit on the shelf, untriggered for your entire life. The trigger is something that sets off the autoimmune issue. Our genes load the gun, but something in our environment or lifestyle creates a stress that pulls the trigger when it comes to chronic disease. These triggers are things like stressful events, infections, and hormone imbalances or changes.
Your genes play an important role in warning you about what health issues you are most at risk for. Armed with this information, you can get a head start on prevention. The question of “nature or nurture,” is the wrong question to ask. It isn’t an either / or question. Nature is your genetics, but your genetics cannot be expressed without the disease being nurtured. This nurturing happens through things like infections, stress, imbalances, toxins, etc. This, is epigenetics.
Primary to understanding the immune system, is understanding where it lives. Roughly 80% of the immune system lives in the gut – the gastrointestinal tract. Sound odd? The gut doesn’t just break down food. New emerging research reveals what the gut does beyond food digestion. When you look at the intestines under microscope, it makes perfect sense that your immune system lives there. Gut health is a key factor in battling autoimmune disease.
Triggers
There are a handful of common triggers. A major trigger for women is pregnancy. Pregnancy is not only stressful on the body but is also a time of sweeping hormonal changes and a major immune system shift that can influence our genes significantly. Naturally, due to hormonal fluctuations, puberty and menopause are also common times in the lives of women for higher rates of autoimmunity to be triggered.
Another common trigger is food. The immune system can start to react in a negative way to food being consumed due to something called “leaky gut.” Essentially, food can be either a good thing and provide necessary, healing nutrients to the body, or it can be a bad thing, giving your body the wrong message and instead feeding disease and causing inflammation. Understanding what you should and should not be eating is of utmost importance when it comes to autoimmunity. Unfortunately, managing autoimmunity is not as simple as a one-size-fits-all diet. Each person’s body can react differently to the same foods. We will go into more detail into how you can determine the best nutrition plan for your body in later chapters.
Leaky Gut
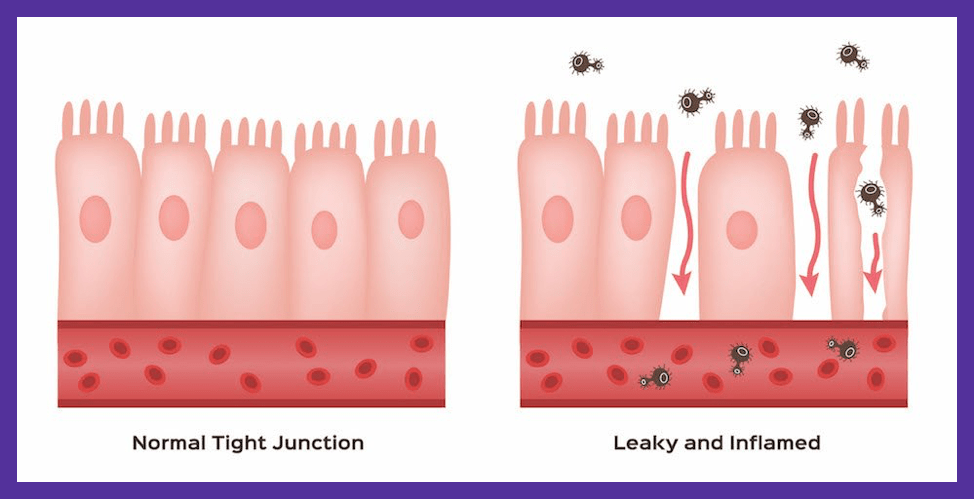
Understanding Autoimmunity: Leaky gut is an integral part of the puzzle in the development of autoimmunity. A breakdown of the barriers that protect you from the outside world is the perfect opportunity for your immune system to become unregulated. This central area of dysfunction, the gut, is at the core of most autoimmune disease. The gut barrier (the wall of cells that surround your gut) has a very important job. By lining your intestines, it is positioned to absorb nutrients from the food you eat and prevent harmful things from going straight into the bloodstream.
On the other side of that wall lives your immune system. Simply put, this is brilliant, because that is right where the majority of our exposure to the outside world happens. That is exactly where the immune system needs to be strongest, combating all harmful matter that enters the body. The immune system is the first line of defense to protect us from things like viruses, parasites, and bad bacteria in water, food, and the environment. The tricky part is, that it isn’t always the most obvious “bad guys” that trigger the immune system to shift into overdrive. Often it is things we “do” and things that we get exposed to daily that play the biggest role when trying to understand autoimmunity.
The Immune System
Great news! You are NOT powerless. The immune system is designed to protect the human body. By definition, autoimmunity is an abnormal response to this brilliantly designed system. However, autoimmunity does not happen without cause. The key to combating autoimmunity is learning those causes and adopting lifestyle changes to reduce key triggers. The effort can make all the difference.
If you have a diagnosis that is affecting a specified location in your body, that means that this area is under attack by your immune system. When unable to identify the source of the issue, a plan can be developed to heal the root cause. If proper course is undertaken, you may see multiple autoimmune symptoms and conditions, that are seemingly unrelated, start to disappear.
Lupus is an autoimmune disease categorized in the same family as psoriasis, multiple sclerosis, and rheumatoid arthritis. You may experience symptoms of any of these disorders.
Start with gut health. Over 70% of your immune system resides in your gut. Fix your gut and you may find that symptoms improve throughout your entire body. Supporting your immune system allows your body to naturally heal and function as it was so perfectly designed to do.
Inflammation
We can’t forget the root of all chronic disease: inflammation. The first thing to understand about inflammation is that not all inflammation is bad. Yes, you heard that right. Inflammation is your body’s natural response to what it perceives as harm or stress, and at the root, inflammation is a healing mechanism. However, when inflammation becomes chronic or doesn’t go away, it becomes harmful and not only perpetuates dysfunction in the body and contributes to symptoms like pain, but can also keep your immune system stuck in overdrive and be a major force in perpetuating autoimmunity.
Inflammation manifests in the body as brain fog, pain, and depression. It can develop from obvious things like diet and environment, but also from hidden things like hormonal imbalances or blood sugar issues, or things that don’t appear as symptoms right away or are difficult to identify. There will be further discussion in later chapters on how to identify inflammation in the body, and means to combat and avoid it.
Inflammation is an underlying factor in most chronic conditions and can also trigger and perpetuate autoimmune conditions. Understanding inflammation, what is causing it, and how to gain control over it are important steps in learning how to heal the body and put autoimmune conditions like lupus into remission.
Complications
Infections are the leading cause of death in lupus patients. People with autoimmune diseases such as lupus can become severely ill from simple, common infections like the flu. This is due partly from the involvement of the immune system but also from commonly prescribed lupus medications. Many of the drugs used to manage autoimmune conditions are immunosuppressants, suppressing the immune system.
With many autoimmune conditions, including lupus, the immune system is overactive. For this reason, the standard treatment is to suppress it, which is the beginning of a vicious circle. Of course, when you suppress the immune system, other issues arise. The immune system is designed to protect you, but by suppressing it you open the door to a whole host of other infectious agents, ones which we normally get exposed to and fight off daily. These infectious agents can cause infections and bring on illness. Lacking a healthy immune system to fight back, people with lupus are more susceptible to poor health outcomes and complications due to infection.
People who are not on immunosuppressants also face challenges with their body’s ability to fight off infections. An overactive immune system, does not necessarily mean that it is effective at fighting off infections. The immune system is like a scale that works when each side can stay balanced with the other. In the realm of autoimmunity, this balance shifts, causing problems with the immune system’s ability to maintain its vital functions.
Other serious complications of lupus involve renal failure and central nervous system (CNS) involvement.
Many people with lupus are diagnosed and suffer the consequences of poor kidney function. Our kidneys are important organs that not only help eliminate waste from our body through urine production, but also help us absorb nutrients, help control our blood pressure, and make sure our cells are getting oxygen and nutrients to function. A majority of the time, kidney dysfunction goes on for years without being diagnosed or caught early enough when it can still be prevented. This can lead to other complications and symptoms in the body that can appear as if they are coming from somewhere else. Something like high blood pressure can be thought of as just a cardiovascular marker when in fact it could be stemming from an underlying kidney dysfunction. If we monitor and catch things early, we minimize symptoms. We can also help prevent life-threatening complications such as renal failure.
Autoimmune destruction and inflammation caused by lupus are known to affect the heart and cardiovascular system. Heart disease is another leading cause of death in people with lupus. According to Johns Hopkins, “the risk of heart attack in women with lupus aged 35–44 is 50-times greater than that of women without lupus.” Stroke, heart attacks, and septic arthritis are common and serious complications of the vascular effects from lupus. People on immunosuppressants have a higher risk of inflammation of the heart, or myocarditis, due to a decreased ability to fight off infections that commonly cause myocarditis.
People with lupus also have symptoms that are not specific to lupus.
These include weight loss, fatigue, fever, blood clots, and hair loss in spots or around the hairline. They may also have stomach pain, heartburn, and poor circulation to the fingers and toes. Miscarriages are common in pregnant women.
The link between autoimmune disease and gut health is key to understanding the complications of diseases like lupus. Start with the health and well being of the gut and you can begin to gain control over things like inflammation, blood sugar imbalances, and upregulated immune systems.
Healthy Regards,
Dr. Tiffany Caplan & Dr. Brent Caplan
PS: Have fun exploring the creative and flavorful recipes in Dr. Caplan’s cookbook “Lupus Friendly Recipes to Calm the Fires of Inflammation.” These delicious recipes are great support for lowering inflammation due to lupus or other autoimmune disease symptoms.


I have had some symptoms that have been concerning me. I know my hormones are not balanced. Hair loss bad digestion pain through the right side of body tingle fingers and toes. Not sure what to do.
Hi Rachel. I’m sorry that you are going through all of this. We’re here to support you on your health journey if you need us. You can reach out to us here: https://caplanhealthinstitute.com/consultation/
Yo tengo epilepsia desde los 5 años tipo “ausencias” he podido trabajar con normalidad pero estoy sujeto a medicamentos que si los quiero dejar no puedo porque son adictivos. Luego a los 65 años he descubierto que soy “Celíaco” por genética ya de nacimiento. También tengo “Hipotiroidismo” desde siempre con Bocio multinodular Granuloso. Pero yo pienso que será un problema entrelazado de la “Celiaquía Permeabilidad Intestinal y Tiroides” Y aqui la medicina en my pais deja mucho que desear.
I am experiencing a sudden onset of numerous ailments and don’t know if they’re interrelated or commence in the gut.
My medical history started generally in 2005 with a heart attack, with three stents placed. Since then I have sustained 7 more attacks and now with 11 stents 15 yrs later–along with the obvious drugs (I wonder if these too have an influence on my gut microbiome).
In April 2020 (last year) I was bent over from stomach pain (could not sit), and the local ER could not discover the cause after a CT scan–(minor liver lesions) –a mystery STILL today!
Currently, my entire gut has been inflamed from the bottom of my ribcage for about a year (I can feel my heartbeat in my lower abdomen); my left ear discharges non-stop a little (four months); my right lips and the tip of my tongue numb up in the morning, then disappears after 20 minutes; and right shoulder (torn rotator) getting progressively worse. The current heart rate is 45 bpm, no HBP (115/70)
My GI doc is somewhat stymied, going for an MRI this week, getting tired of telecalls. At 67, I feel like I’ve been steadily falling apart this past year…I don’t want to think bad thoughts about all this
I’ve ordered your videos to understand a little bit more, and maybe assisting in asking my GI doc (and cardio) the right questions, or perhaps even pointing them in the right direction. So I am appreciating your work and more modern approach. Thank you.