Lupus, known as the invisible disease, is challenging to properly diagnose because of how differently it affects each person. Our mission is to shed light on this devastating disease and present a realistic path to a healthier, more livable future. It is possible to reclaim your life and regain your health. It begins with understanding the facts about the illness and learning how to control your journey.
A diagnosis of lupus is not to be taken lightly. It’s a serious disease affecting many parts and systems of the body, often leading to serious and sometimes life-threatening complications. Like other autoimmune conditions, symptoms develop gradually so it can take years to recognize that symptoms are abnormal and often many more years to finally receive a correct diagnosis and answers or solutions.
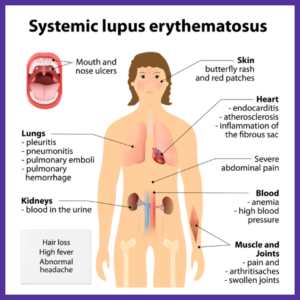
Systemic Lupus Erythematosus is a multi-system autoimmune disease.
Because it usually affects many different body parts (joints, skin, and/or organs) and presents a wide range of complications and symptoms (many of which can be fatal), no two individuals have the same disease process. It is difficult to treat because each person deals with a variety of different and often unrelated issues.
Life-threatening conditions can develop rapidly, and patients need to be monitored closely and often for any changes. Functional laboratory testing can offer hope and is an effective tool for monitoring and detecting changes before complications set in.
Lupus Diagnosis.
To fully understand the complexities of this illness, it first helps to understand a couple of basic things. Unfortunately, over 63% of lupus patients experience being incorrectly diagnosed. Before reaching a correct diagnosis, 50% of patients end up searching for answers from four or more different healthcare providers. It is a long, exhaustive process to get to the bottom of the problem and finally start to uncover some solutions.
If you ask a person with this condition sufferer when things started to change and their health made a turn for the worse, they can usually pinpoint a turning point in their lives, when they started to notice abnormal symptoms – fatigue for no reason, joint pain, mood changes, or feeling “just not themselves.” While usually gradual, these changes can often be traced back to a stressful time or event. For some people, symptoms come on more suddenly, or sometimes, seemingly out of nowhere. One day they were fine and the next day they were experiencing pain, heavy fatigue, or a sudden butterfly rash.
Most symptoms small, subtly. You may notice your joints bothering you while walking up steps, or it just gets hard for you to make it through a full day. You may experience weight gain without changing your eating or exercise habits. These symptoms, that seem small, are usually the first attempts of your body to tell you something is wrong. The main issue is, most people and their doctors don’t start to take these issues seriously until they begin to worsen.
Lupus is not an infection or a type of cancer.
It is an underlying problem causing the immune system to attack the body instead of protecting it. It is also known as “the great imitator.” Symptoms vary and can mimic many other diseases and conditions. You cannot “catch” lupus from another person, but you can certainly have a genetic predisposition if it runs in your family.
Even if you monitor your systems and recognize that something is wrong earlier on, many doctors check only a limited number of lab markers associated with the particular symptoms or systems that the person is experiencing issues in. This creates an issue with catching things early and before the complications worsen.
Appropriate and thorough testing is essential in treating and managing lupus. Testing needs to cover a wide look at the body as a whole instead of different pieces or parts. To get full testing, you can turn to functional medicine. Functional lab testing and evaluation go above and beyond the standard markers and allow a deeper look at what is going on in all systems of the body to view the interconnected web that makes up the whole person. We know the body does not operate as a bunch of separate and individual body parts or systems. So Why are we being tested and treated as if we are?
Standard guidelines have been set for requirements for diagnosis.
Diagnosis is based on multiple criteria, and standard guidelines have been set for requirements for diagnosis. Diagnosis is based on two main components: symptoms or clinical presentation and laboratory findings. In order for diagnosis to be made, a minimum of four out of eleven criteria must be present. The more positive the criteria, the more confident the diagnosis.
There are “clinical criteria” and “immunologic criteria,” and in order to diagnose lupus, a person must meet at least one criterion in each of those two classifications as part of the minimum. It is possible to have lupus and not have four or more of the diagnosis criteria. Then again, someone with another condition such as rheumatoid arthritis can meet the criteria and not have lupus. The criteria are good guidelines but are not always 100 percent of the picture.
Lupus is a complex disease. Simple changes can effect change and lead to managing your immune system. Changes may manage many symptoms that prevent a healthy, enjoyable life. The typical path of the illness is one of pain and suffering. It is possible to achieve a different, healthier reality by changing one’s approach to health and self-care. Everyone deserves a chance to control the fate of their health and happiness. Remission IS possible.
Different Types of Lupus
The general term lupus refers to SLE; however, there are multiple forms under the greater umbrella of diagnosis. While a majority of cases have systemic involvement and affect multiple body parts or organ systems, some forms of affect only a specific tissue, such as the skin. And while most forms of lupus tend to have lifelong implications, some forms cause only temporary or short-term effects.
Neonatal lupus refers to the development of lupus in a newborn who is born to a mother that has lupus. This is a rare disease when the mother’s lupus antibodies affect the developing fetus, leading to rashes and/or heart damage.
Cutaneous lupus refers to the involvement of the skin. This can occur with or without the systemic form of lupus (SLE). Roughly 10 percent of lupus cases affect only the skin without other systemic involvement. The classic example of cutaneous lupus is the symbolic butterfly rash across the nose and cheeks. Around 25 percent of people with the systemic form, SLE, will also have skin involvement.
Discoid lupus refers to a type of cutaneous lupus that causes disc-shaped rashes that most commonly affect the head, face, and ears. These round rashes can cause permanent discoloration of the skin and damage to the hair follicles. When discoid lupus affects the scalp, it can cause areas of irreversible hair loss. Fortunately, most people with chronic discoid lupus do not develop the systemic form.
Drug-induced lupus refers to a syndrome that presents as SLE, but as the name suggests, it is caused by a reaction to certain medications. Drug-induced lupus can present clinically identical to SLE, but the symptoms go away once stopping the medication that caused it.
Epidemiology of Lupus
According to the National Resource Center on Lupus, more than 16,000 new cases are reported every year in the United States. Estimates show that at least 1.5 million Americans suffer from lupus and the rates may be higher due to many people who remain undiagnosed. Worldwide, lupus affects approximately over 5 million people.
Lupus is two to three times more prevalent among women of color — Hispanics/Latinos, African Americans, Native Americans, Asians, and Pacific Islanders — than among Caucasian women. Recent research indicates that lupus affects about 1 in 537 young African American women. And African American patients are more likely to have organ system involvement, more serious complications, and higher rates of mortality.
The lack of public information and awareness may be a factor in the struggle to get accurately diagnosed. People age eighteen to thirty-four are the highest risk demographic for developing lupus. And yet over 72 percent of eighteen-to-thirty-four-year-olds have never heard of or know little of the illness beyond the name.
With lupus, many times, multiple tissues, organs, or systems are affected, and the symptoms aren’t always easy to connect the dots or pinpoint the problem. Because patients can present with a wide array of symptoms that don’t seem to be connected, healthcare providers may think multiple different diseases or conditions are present simultaneously when in fact, the symptoms may all be able to be traced back to “the great imitator.” This may contribute to the reason it takes on average over seven years and four different healthcare providers to come to the diagnosis of lupus.
One in three people diagnosed also suffers from multiple other autoimmune diseases.
Other common autoimmune diseases include Sjogren’s and Hashimoto’s. Sjogren’s affects the mucous membranes of places such as the eyes, mouth, and nose. People with Sjogren’s experience extreme dryness in those areas, which can lead to other issues.
Hashimoto’s is an autoimmune disease that causes an attack and destruction of the thyroid gland leading to symptoms of hypothyroid or low thyroid. Symptoms of low thyroid include things like fatigue, insomnia, hair loss, constipation, and depression. Many symptoms associated with an autoimmune diagnosis can overlap, thus making it that much harder to pinpoint the cause of the symptoms and causing doctors to just chase the symptoms with medications.
Healing is a Journey
Many people suffering with the illness would agree that while symptoms such as pain and fatigue have a negative impact on their daily lives, the frustration that comes with this disease may far outweigh the physical symptoms. A lot of the frustration stems from misunderstanding the disease as a whole. Most people are diagnosed after years of suffering from a wide array of different seemingly unrelated symptoms. Many times, these people have been repeatedly told their labs are normal and there is nothing wrong, leading them to believe that their symptoms are “normal”—simply a result of age or stress.
But they are not normal. Once you receive your diagnosis, you can heal by committing to lifestyle changes. Healing is a journey and requires changes on your part. The long-term benefits of making necessary changes far outweigh the short-term hardship of making those changes. And the more you practice better habits, the better you feel and the easier it becomes.
When receiving a frustrating diagnosis…
While receiving your diagnosis is frustrating, the even more frustrating part is a lack of understanding from loved ones, friends, and even doctors. When you have a disease like systemic lupus erythematosus that can attack random tissues in your body and your symptoms show up as a whole range of seemingly unrelated issues, not only is it hard to explain what you are dealing with, but it is also hard for others to relate and even harder to get the correct diagnosis in a timely manner. How do you explain to someone how it feels to feel your body falling apart when they have never experienced anything similar before? That lack of understanding can seem isolating and one of the hardest parts of being diagnosed.
Healthy Regards,
Dr. Tiffany Caplan & Dr. Brent Caplan
PS: Have fun exploring the creative and flavorful recipes in Dr. Caplan’s cookbook “Lupus Friendly Recipes to Calm the Fires of Inflammation.” These delicious recipes are great support for lowering inflammation due to lupus or other autoimmune disease symptoms.
PPS: Self-care is so important, and an essential component of conquering autoimmune disease. This is why my wife; Tiffany and I created the “Simple Self Care for Autoimmunity” e-book. This guide provides 8 simple and effective ways to practice self-care you can start today! It’s our gift to you! Download it now at no cost!


I have Lupus and several other autoimmune disorders. Many symptoms CAN NOT be figured out by doctors which is Overwhelming Frustrating. Also appears that my endocrine System is Shot. I’m fatigued beyond belief and no one understands of course. My mind is so foggy that I feel as if my head is full of helium and it’s debilitating although I try to hide this symptom. I’m in desperate need of help as I’ve gotten to the Point that Life isn’t worth living if it’s going to continue to be this way. I also feel as if I’m drugged. Never took illegal drugs so that’s an assumption. I also have the Mutated MTHFR Gene which affects the way I absorb medications and possibly nutrients. PLEASE HELP ME.
I’m sorry that you are going through all of this. It can be tough dealing with a debilitating condition but you are not alone. I would encourage you to join our lupus and autoimmunity Facebook support group. A great place to start is with an elimination diet to determine any food sensitivities that may be flaring up lupus. There are resources on this within the Facebook support group. I’ll also post below a link to our self care guide for autoimmunity. These are some great places to get started. We are also here for you for additional support in your health journey. You can reach out to us here, to work with us: https://caplanhealthinstitute.com/consultation/
Resources:
Facebook Lupus & Autoimmunity support group: https://www.facebook.com/groups/2396443747235585/?source_id=2066251227006518
Self Care Guide for Autoimmunity: https://caplanhealthinstitute.com/self-care-autoimmunity/
Hi Cathy,
I can relate to your story although I did not receive the lupus diagnosis, only a vague expression that “something” inflammatory is happening but like you, they can not figure out my symptoms. I have had days with that same drugged feeling you described. My rheumatologist said she had not heard anyone describe that symptom. She said she didn’t know how to help other than to recommend getting off gluten and sugar. It was the best advice! I got such good results that my doctor had me do food sensitivity testing which eliminated so many symptoms. I know it’s hard when the specialists aren’t able to help you, but there’s a journey you can take without them as the doctor described to you. It has made a world of difference in my symptoms, and ultimately left me in a place where I am not worried about WHAT is wrong with me, but what steps I can take each day to improve my health. Good luck in your healing journey!